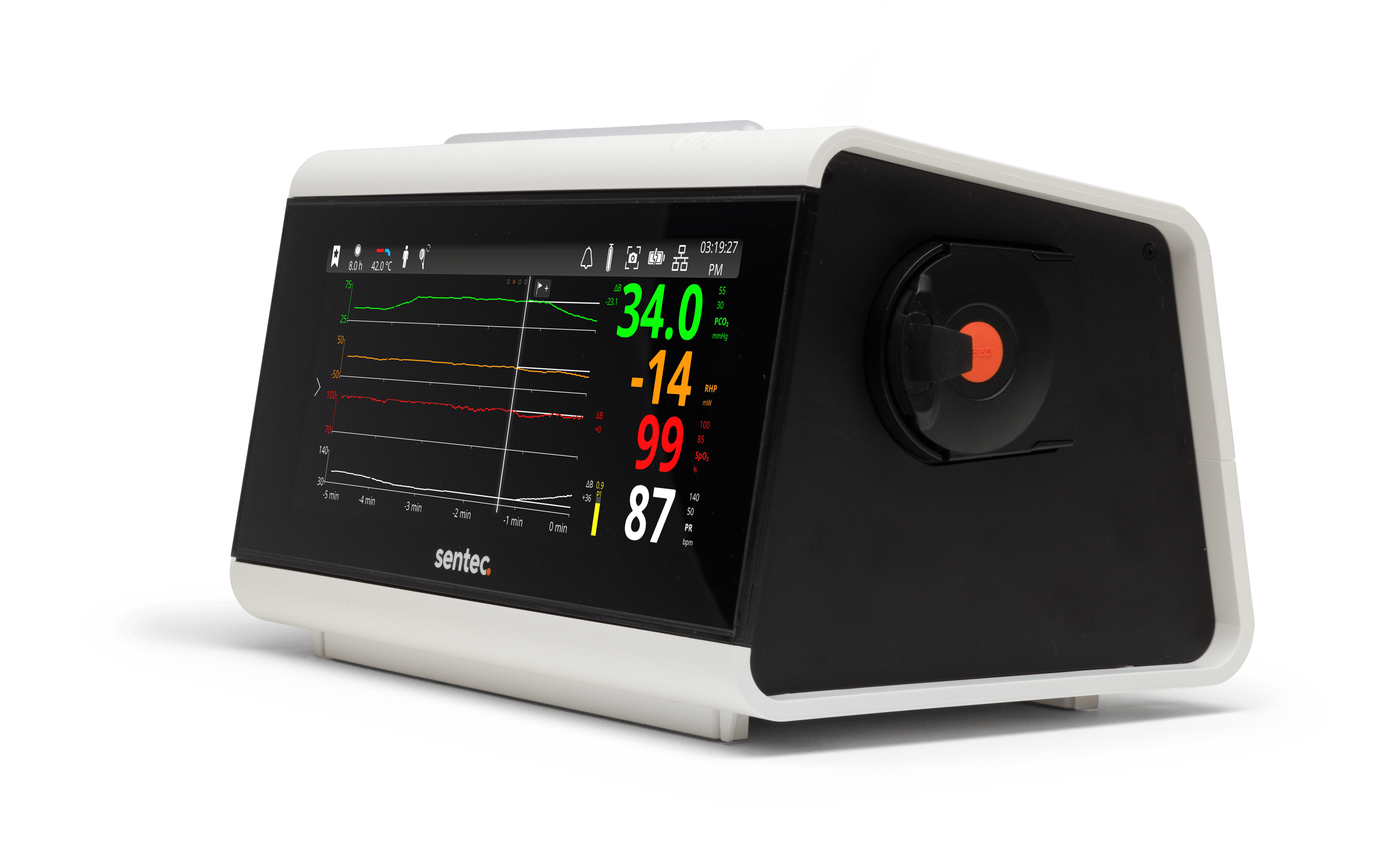
TRANSCUTANEOUS MONITORING (TCM)
Continuously monitor gas exchange noninvasively
Continuous, accurate tcPCO2 and SpO2 values add to the clinical picture without additional lab draws on patients regardless of ventilation method.
ELECTRICAL IMPEDANCE TOMOGRAPHY (EIT)
Assess regional lung function at the bedside
Real-time regional lung function images inform ventilation strategies to help clinicians personalize care and achieve optimal outcomes.
Guide ventilation in real time without repeated blood gases
Accurately assess ventilation on any form of respiratory support


Deliver less invasive, customized patient care

Deliver personalized respiratory support

Guide ventilator settings
Guide ventilation in real time without repeated blood gases
Accurately assess ventilation on any form of respiratory support

Deliver less invasive, customized patient care

Deliver personalized respiratory support
Guide ventilator settings

Deliver less invasive, customized patient care
Benefits for Patients
Benefits for Providers
Benefits for Facilities
Explore TCM Products & Support
Learn more about transcutaneous monitoring technology or view our product resource library to support an existing system.
IPV THERAPY IN ACUTE RESPIRATORY CARE
The trusted solution for secretion clearance, hyperinflation relief, and lung recruitment
Sentec IPV Therapy is an effective, safe, and well-tolerated airway clearance therapy that utilizes the unique Phasitron delivery interface to restore gas exchange capacity across diverse patient populations and delivery interfaces.
IPV THERAPY IN ACUTE RESPIRATORY CARE
The trusted solution for secretion clearance, hyperinflation relief, and lung recruitment
Sentec IPV Therapy is an effective, safe, and well-tolerated airway clearance therapy that utilizes the unique Phasitron delivery interface to restore gas exchange capacity across diverse patient populations and delivery interfaces.

Benefits for Patients
Benefits for Providers
Benefits for Facilities
EIT IN ACUTE RESPIRATORY CARE
Informed care for complex critical care patients.
Regional lung function monitoring provides clinicians with relevant clinical information about a patient or intervention.
Availability of the LuMon™ System is dependent on country and product version. The LuMon™ System is currently available for investigational use only in the United States. Request information below to be notified of availability in your area.
EIT IN ACUTE RESPIRATORY CARE
Informed care for complex critical care patients
Regional lung function monitoring provides clinicians with relevant clinical information about a patient or intervention.
Availability of the LuMon™ System is dependent on country and product version. The LuMon™ System is currently available for investigational use only in the United States. Request information below to be notified of availability in your area.

Benefits for Patients
Benefits for Providers
Benefits for Facilities
Explore EIT Products & Support
Learn more about electrical impedance tomography or view our product resource library to support an existing system.
Transcutaneous Monitoring: Why CO2?
This animation offers a simple explanation for why [...]
Transcutaneous Monitoring: Why CO2?
This animation offers a simple explanation for why [...]